Clinical skills sessions, like many things, went virtual when COVID-19 shut down in-person teaching at the Island Medical Program. While the move kept everyone safe, it took away the space for students to practise with a volunteer patient.
“Clinical skills don’t easily translate online,” says Robin Stone (IMP Class of 2024), noting that social distancing protocols also made it difficult for students to practise with each other in between sessions and before exams.
But Robin saw an opportunity in the situation. Drawing on her previous experience and connections in the tech industry, she led the development of an app that allows medical students to conduct GI, Cardiac, and HEENT exams with a virtual patient.
The Clinical Skills Digital Practice Tool (learnclinicalskills.ca) uses natural language processing (NLP) artificial intelligence to bring the assessments to life. When students type in their questions and instructions, the app responds with photos, audio (e.g., heart beats), and written descriptions. “There’s a vast amount of content, a lot of which was created by other medical students” says Robin of the programming behind the app. “There may be 30 different ways to ask ‘Can I see your eyes?’ and we needed to program them all.”

(L-R) Ena, Bao, and Naydia volunteered as patients for the Clinical Skills Digital Practice Tool.
Though the communication is artificial, the media and the featured patients are real. Students have the opportunity to practise with three different volunteers – Ena, Bao, and Naydia – who are of various ages and backgrounds. “It was important the app have BIPOC representation,” Robin says. “Students need to learn what ‘normal’ looks like for different people.”
The app runs just like an in-person clinical skills session. After choosing their patient and exam, students enter instructions and report their findings in the app until they believe they have completed all the required actions. Then the apps shows all of their actions and reports alongside the system’s answer key so students can see which of their actions were asked correctly, if they missed any actions according to best practice exam steps, and how their responses compare to the answer key.
“This is an innovative project,” says Dr. Laura Farrell, who acted as the UBC faculty project lead and helped Robin apply for the $75,000 UBC Strategic Investment Fund grant that financed the app (and for which Robin was the first student recipient). “It met an important need as the COVID pandemic resulted in students not being able to have the same in-person clinical skills experiences or to practise their clinical skills on actual patients. Robin brought skills and knowledge from her past experiences and built a great team who I felt privileged to work with and to learn from.”
Though clinical skills are running in-person again, Robin says students can still use the app to supplement their live training sessions and to practise for the OSCEs. It provides a safe virtual space for student to hone their skills and practise the order of their questions before they meet a real patient so they can “really focus on the patient in the room during an exam.”
“The students who have used it loved it,” she says, adding she hopes more students will take advantage of the app.
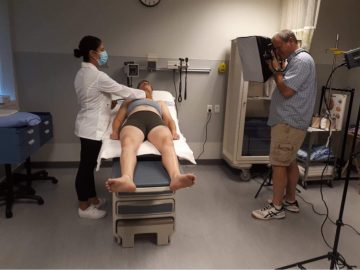
Though the app’s communication is artificial, the media and the featured patients are real.
The development team hopes to soon make the app even more lifelike by including video of the volunteers and text-to-audio technology, which would allow the chat bot responses to be spoken instead of written. Robin says they also plan to add a pathology feature, in which the virtual patients will have a complaint that students need to decipher.
Robin and her team wrote a paper on the project, which was accepted into Medical Education and will be published in the journal’s “Really Good Stuff” section this November.