When volunteering as a first responder in her remote hometown of North Shuswap during a major heatwave, Simona Bene Watts (IMP Class of 2024) noticed something worrying: bystanders were often not performing CPR on cardiac arrest patients by the time she and other first responders arrived.
An estimated 35,000 cardiac arrests occur in Canada each year and a majority of those happen outside of a hospital. According to the Heart & Stroke Foundation of Canada, less than 10 per cent of people who suffer an out-of-hospital cardiac arrest live. However, survival rates double if someone receives CPR and automated external defibrillator (AED) treatment, and people who get help earlier have the best chance of survival and a functional recovery.
Still, many rural and remote communities experience long wait times for emergency health services, which results in worse cardiac arrest outcomes compared to their urban counterparts. This makes having bystanders who know how to perform CPR and use an AED in these communities vital.
Lack of training is often a reason why bystanders do not carry out these live-saving tasks. “In the weeks following the heatwave, I reflected on the situation and the barriers for rural community members to receive CPR training,” Simona says. “CPR is not part of the BC secondary school curriculum. To seek training, individuals have to pay out of a pocket and often have to travel more than an hour to attend a CPR course.”
As she began looking for solutions, Simona recognized she had resources she could mobilize. “I was surrounded by a group of knowledgeable medical students who would make excellent CPR instructors, as well as by medical training equipment located at Island Health’s Centre for Interprofessional Clinical Simulation Learning (CICSL), the Heart & Stroke Foundation, and St. John Ambulance that we could borrow to make a uniquely low-cost course for rural and remote communities,” she explains. “From this, the idea of the Rural CPR Outreach Project (RCOP) was born!”

(L-R) Simona Bene Watts, Nick Wilson, Erin McDonagh, and Wesley Richardson on their 2022 RCOP tour.
After securing sponsors to cover their course, equipment, and travel costs, the RCOP team – Simona, Erin McDonagh, Wesley Richardson, and Nick Wilson (all IMP Class of 2024) – headed up Island in 2022. They taught the Heart & Stroke Foundation Hands-only CPR training guidelines to more than 300 students in Sooke, Campbell River, Port McNeil, and Port Hardy during the project’s first year.
As the RCOP is a FLEX project, supervised by UBC clinical professor Dr. Kevin Shi, the IMP facilitators also gave their students pre- and post-course surveys to help them evaluate the effectiveness of the program. They found that students’ CPR knowledge improved from 48 to 90 per cent and that students’ perceived comfort performing CPR improved from 40 to 85 per cent.
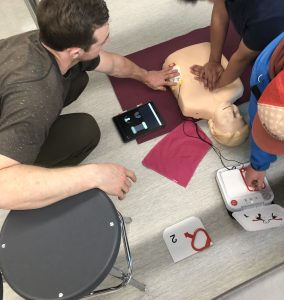
Nick helps students with compressions and AED placement.
“Not only are we equipping youth with life-savings skills, but we are also offering them an opportunity to interact with medical students face-to-face and learn more about medical education and health professions,” adds Simona. “It’s no secret Canada needs more doctors, especially in rural and remote regions, and we believe that empowering youth to pursue a career in medicine starts with exposure to medical experiences like our course. In addition, many of our RCOP team members are from rural and remote communities themselves and they believe that if they had had the opportunity to meet and create mentorship connections with medical students, it would have eased their own path to medical school and would have encouraged others to pursue such a career.”
After last year’s success, the RCOP team is excited for its second year of workshops to start this April. The tentative 2023 itinerary includes visits to Sooke, Salt Spring Island, Ucluelet, Campbell River, Quadra Island, Port Hardy, Port McNeill, and Powell River.

Simona sits with equipment.
Simona says they are also already looking to the future of the program. The team has expanded to include eight IMP students, spanning Years 1 – 3, and it has an active mentorship progression in place so students at the beginning of their medical training will learn the skills needed to carry on the project for years to come. New members Alison White, Jocey Terwoord, Margot Schmidt (all IMP Class of 2025), and Ethan Schovanek (IMP Class of 2026) will take on the role of teaching classes this year. Simona says the team would also like to expand the program to even more communities around Vancouver Island and plan to apply for the BC Ferries Community Travel Support Application to reach some of these more remote communities. They are also discussing the possibility of adding Naloxone overdose response training to the program. “We will provide a brief overview of the theory of how to use Naloxone and where to access Naloxone kits in the community,” she says. “But we are taking time to research how to teach this skill effectively and as safely as possible.”
Students at the Southern Medical Program and Northern Medical Program have also expressed interest in expanding the RCOP to their regions in upcoming years.
The IMP RCOP team would like to thank its sponsors over the past two years: the Island Medical Program, CICSL, the Heart & Stroke Foundation, Victoria St. John Ambulance, and the Rural Health Services Research Network.